How To Improve Mental Health Services In Malawi
There are reports that mental illnesses are common and that more than 25% of people globally suffer from mental disorder in their lifetime. The treatment gap recorded between poor and rich countries is estimated to be between 30-50% in developed countries and 7685% in developing countries. The World Health Organization (WHO) reports that higher income countries have more facilities and higher utilization rates than low and middle income countries (LMIC).
The global median of mental health facilities per 100,000 population is reported at 0.61 outpatient facilities, 0.05 day treatment facilities, 0.01 community residential facilities, and 0.04 mental hospitals. In Malawi, there are many people suffering from mental health conditions but have no access to care due to several reasons including: centralization of mental health services and the disintegration into primary healthcare; there are very few mental health professionals in the country and the general health care workers have no competency for handling mental health conditions; inadequate resources are allocated to mental health care; and high levels of societal stigma towards people suffering from mental health issues. Below we will list some burdens to Mental Health in Malawi and the right solutions.
Shortage of Mental Health Personnel
Malawi’s public health system follows a three-tiered system of medical facilities:
- Urban center hospitals and other specialized hospitals (tertiary)
- District hospitals (secondary)
- Health posts, health centers and community and rural hospitals (primary).
However, the health budget prioritizes allocating resources to the top tier of health services; other tiers are often without supplies – particularly primary care facilities. Furthermore, there are less than 100 registered doctors and 3000 nurses to service all three tiers of the health system, and there are no doctors and few nurses at the district tier.
Low capacity of primary health care workers
Many of the health workers in Malawi are not equipped them with necessary knowledge and skills as well as resources, to aid to presentation of correct diagnosis to in turn free up not only financial resources, but also staff time. There is need to among other things; support in-service training, support the human resource department for health and specific training in mental health services integration and encourage mentorship and strengthen supervision.
The above stated are among the top ranking burdens to mental health in Malawi. The understanding of MHL has expanded in recent years from its original definition of “knowledge and beliefs about mental disorders which aid their recognition, management and prevention” to a more comprehensive framework, grounded in the World Health Organization approach to health literacy, to encompass:
- Enhancing capacity to obtain and maintain good mental health.
- Enhancing understanding of mental disorders and their treatments.
- Decreasing stigma related to mental illness.
- Enhancing help-seeking efficacy.
Malawi records of an estimated 2000 suicides each year, the lifetime risk of schizophrenia and bipolar illness in Malawi is around 1% and in 2002 and estimations made by WHO that depression was the 4th leading cause of disability in Malawi coming after HIV. Malawi’s the lack of appropriately trained health providers in community health settings makes access to effective mental health care for young people with Depression challenging.
Depression and anxiety affecting up to 30% of mothers bringing their infants to a child health clinic. The children of these women who are likely to have impaired growth and statically up to 28% of patients attending primary care have a common mental health problem with most of them being erroneously diagnosed as malaria and musculoskeletal pains. In addition, HIV/AIDS is associated with a range of mental health problems including dementia, organic psychosis, depression and substance misuse. Depression, that has been left untreated negatively impacting quality of life and future vocational achievement significantly, leading to increased morbidity, contributing to early mortality, and recognition as a potential risk factor for other illnesses.
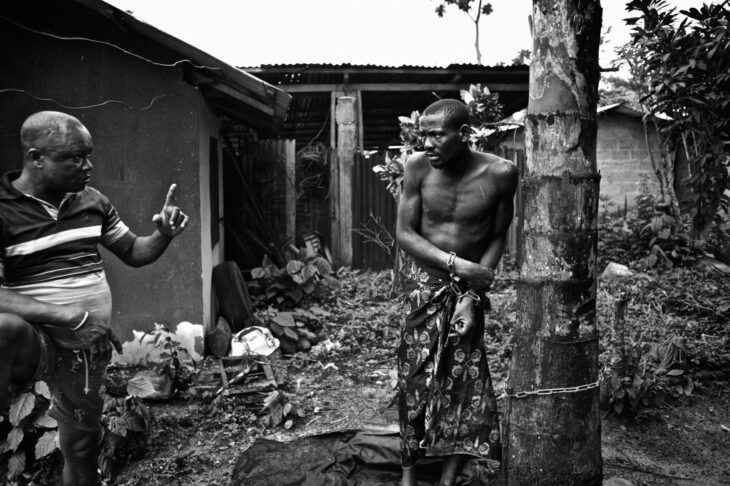
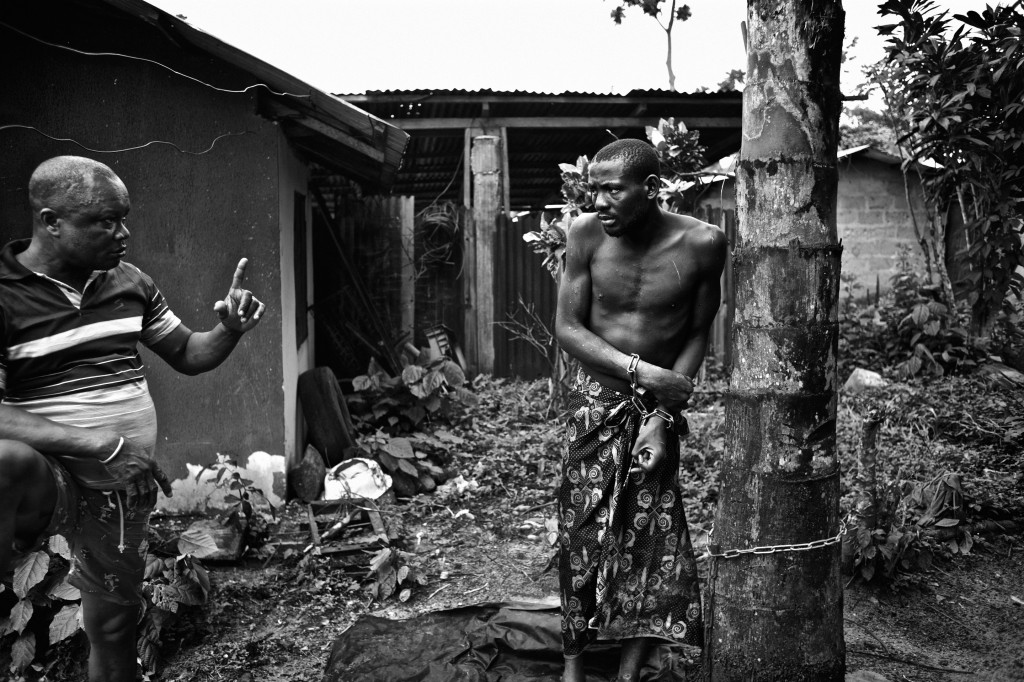
The traditional picture of mental illness is the very disturbed, possibly aggressive, half-naked man uprooting crops, burning houses, or walking down the white line on the road to Blantyre. Such a person would be regarded with fear and either be avoided at all costs, or strenuously restrained and handed over to the police. Yet there have always been other presentations of mental disorder – the silent, withdrawn individual, the child running off into the bush, the adolescent who almost unnoticed begins to lose concentration and fail at his studies. Most people will also recognize mental handicap and make allowances for those who cannot learn as quickly as their normal peers.
Several studies note that traditional care providers are preferred over “orthodox” clinics, often due to cultural influences and a lack of awareness of psychiatric services. Strategies to improve public knowledge and attitudes about mental health and illness, Just as people have always recognized the most mentally disturbed in the community, so traditional treatments have been available as long as there have been traditional healers.
Even those people whose mental disorder present with physical symptoms anxiety and depression, for example: not only need therapy but also a ready and willing health personal during any primary health care service. The explanation for illness in the traditional healer’s approach has influenced the community behavior, attitude and stigma which affects the lives of those with a mental disability today as it has always done. So from the beginning there has been a limited recognition of mental disorder and an attempt by the community to deal with it.
Therefore, Malawi’s Mental Health facilities such as Zomba Central Hospital, Kamuzu Central Hospital and Mzuzu Central Hospital should be staffed with adequate mental health personnel and communities should be sensitized on Mental Health Education and discouraged from seeking help from traditional healers and Dr. Google.
NOTE: Alcohol abuse, recreational drug abuse, are also a big reason why Malawi has had an increase each year for the past 5 years in mental health patients. We will have a special article that covers exclusively how mental illness and alcohol/drug abuse are directly related especially here in Malawi.
Who to contact if you need Mental Health Support In Malawi
NOTE: list of Malawi mental health service providers
St John of God Mental Hospital in Lilongwe(Area 43)
Phone:+265 992 460 253 and also, +265 992 460 254
Email: [email protected]
St John of God Mental Hospital in Mzuzu
Phone: + 265 1 311 690 and also, +265 1 311 495
Email: [email protected]
Zomba Mental Hospital
Phone: +265 1 524 750 and also, +265 1 524 344
Contact Grace Khonje
Licensed counselor, therapist and psychologist. She will gladly help you with any questions regarding how to get more Mental support in Malawi.
Phone: +265 888 664 363
Email: [email protected]
Remember to like our facebook and our twitter @malawibusiness for a chance to win a free Samsung Galaxy Phone on December 25.
You might also enjoy reading about Why does Malawi Fail to Improve It’s Health Services?
- Social & Economic Inequalities in Malawi Today - November 16, 2021
- Cost of education in Malawi - June 11, 2021
- The Quest for a Pragmatic Economic Management Framework in Malawi - February 10, 2021